
views
Diagnosing Vaginal Infections

Recognize the symptoms of BV. Bacterial vaginosis is typically marked by certain symptoms. These include: Vaginal discharge with an unpleasant odor, often described as “fishy.” Vaginal discharge that is white or grey and may look foamy. Burning during urination. Itchiness and irritation around the vagina. Keep in mind that not all women with BV have symptoms.

Recognize the symptoms of a yeast infection. Yeast infection symptoms can often resemble the symptoms of BV. These symptoms include: An abnormal vaginal discharge. The discharge can be a watery, white discharge to a thick, white, and chunky discharge. This is often described as looking like cottage cheese. Itching and burning of the vagina and labia. Painful intercourse. Painful urination. Redness and swelling of the area just outside of the vagina.

Recognize the symptoms of trichomoniasis. Symptoms of trichomoniasis (sometimes called “trich”) in women can be: Vaginal discharge that is usually smelly. Vaginal discharge that is typically frothy or foamy. Vaginal irritation. Yellow or a gray-green discharge. Painful urination.

Keep track of your menstrual cycle. Vaginal infection symptoms can differ depending on where a woman is in her cycle. This is because the hormonal changes during the menstrual cycle can affect the composition of the bacteria in the vagina and the characteristics of the vaginal environment. Knowing your menstrual cycle will help you keep track of changes that you’re experiencing.

Realize that some women experience no symptoms. Many women have BV but they do not have any of the tell-tale symptoms. The same is the case for trichomoniasis. If you suspect you might have an infection, see your doctor. Trichomoniasis can be transmitted to sexual partners. If you suspect you have trich, see your doctor for a diagnosis and treatment.
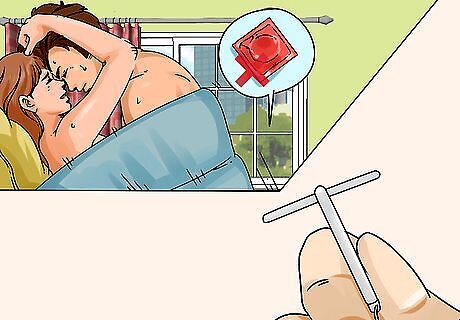
Know that the risk of BV increases with certain activities. Most women have probably had at least one experience with BV. There is no specific cause. Essentially anything that disrupts the normal bacterial balance in the vagina can result in BV. The risk of BV increases with: Having a new sexual partner. Having multiple sexual partners. Having sex without a condom. Douching. Using an intrauterine device (IUD) as a method of birth control.
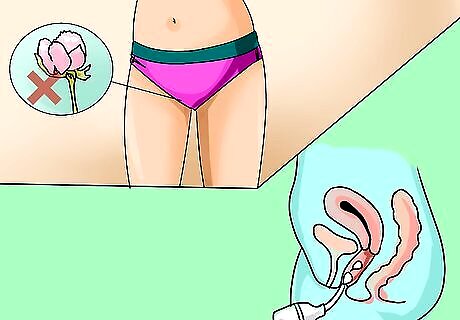
Know what increases the risk of yeast infections. Yeast infections, also called candidiasis, are increased by: Wearing tight underwear or non-cotton panties. These styles of panties can increase the temperature and moisture levels around the vagina and can be irritating. A weakened immune system. Using vaginal douches and/or perfumed feminine hygiene sprays. Specific health conditions (e.g., diabetes).
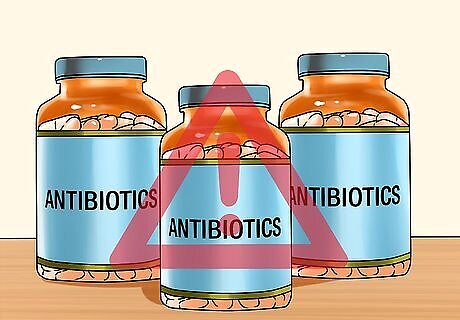
Understand how these vaginal infections can occur. These types of infections can occur because of a number of causes. In BV, there is no specific cause, but it typically results from an imbalance of the normal bacterial populations. Yeast infections can result after antibiotic use; the antibiotics kill off the normal bacterial populations, allowing the yeast to get a “foothold.” They can also come about as a complication of diabetes or during hormonal changes, including a normal menstrual cycle or the use of birth control.

Visit your doctor. It is important to get the correct diagnosis from a doctor before starting treatment. The treatments for the different forms of vaginal infections can be different, depending on the degree of infection. At the doctor’s office, your physician will likely take a sample of the vaginal discharge, ask for a urine sample, and perform a vaginal exam. This exam may be uncomfortable but it is usually over quickly. The discharge will be tested for the presence of bacteria, yeast or other organisms such as trichomonas. It’s important to get a specific diagnosis from your doctor. The approaches for treating vaginal infections differ depending on the type of infection.
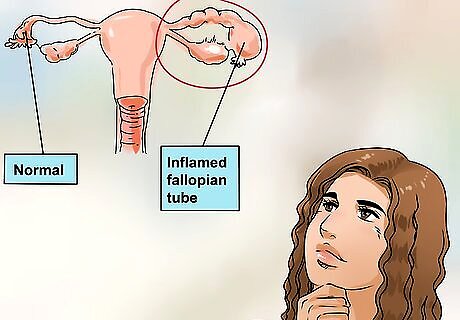
Know the risks of leaving an infection untreated. Untreated or incorrectly treated BV can result in complications such as pelvic inflammatory disease (PID), pre-term births, low-birth-weight babies, and a higher risk of sexually transmitted infections such as chlamydia and gonorrhea. Untreated or incorrectly treated Trichomonas infections can also lead to an increased risk of HIV.

Tell your doctor you’re planning to use natural treatments. You should always get a diagnosis from your physician when you first start experiencing any of the symptoms. This is because some natural treatments work better for BV or candidiasis, and others may not work as well. You can also use these treatments along with the medications prescribed by your physician. They don’t interfere with oral antibiotics. Tell your doctor that you are using these approaches. If you are successful, perhaps your physician can recommend the method to others.

Warn sexual partners if you suspect you have trichomoniasis. Trichomoniasis is classified as a sexually transmitted infection (STI), so if you are diagnosed with trichomoniasis, you should inform any sexual partner so they can be treated as well. If trichomoniasis is the diagnosis, then home remedies are not appropriate.
Treating Vaginal Infections

Treat a yeast infection with a boric acid suppository. Boric acid can be irritating, so you shouldn’t make your own suppository. Do not directly apply it to the vagina. Instead, fill size 0 gelatin capsules fully with boric acid powder; then, insert it into your vagina nightly for 2 weeks. You must not be the recipient of oral sex while using boric acid because boric acid is poisonous to your partner.

Get an over-the-counter gel or cream. Most of the gels and creams for vaginal yeast infections that you can get over-the-counter are almost as effective as anti-fungal medications. Examples include Monistat and Gyne-Lotrimin. Use as directed. If you have recurrent infections, use for seven days.

See your doctor about recurring or long-lasting vaginal infections. If you keep getting vaginal infections or your infection won't go away, make an appointment to see your doctor. Recurrent (or “complicated”) yeast infections often occur in tandem with serious underlying disorders such as diabetes or HIV. If your symptoms don't clear up after three days, talk with your doctor about taking medication. You should also see your doctor if your symptoms return or worsen. Your doctor may prescribe an anti-fungal medication to manage the recurring infection. You will likely need to take this medication every week or month for six months.

Take antibiotics for BV and trichomoniasis. Treatment will depend on the type of infection, how extensive or severe it is, and how long you have had the infection. Antibiotics are prescribed for BV and for trichomoniasis, but they are not effective on yeast infections. BV is generally treated with either metronidazole or clindamycin. These are considered safe if you are pregnant. Male partners usually don’t need treatment, but female partners should be informed and tested. Trichomoniasis is usually treated with a single dose of either metronidazole or tinidazole. These are considered safe if you are pregnant. Trichomoniasis is a sexually transmitted infection, so make sure your sexual partner(s) are treated as well and wait for seven days after treatment to have sex.
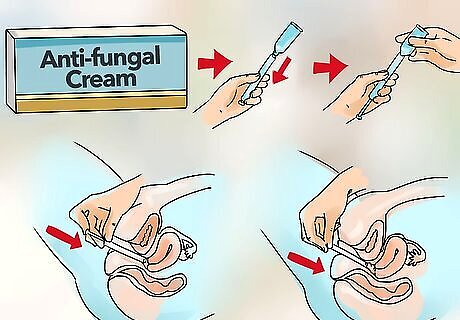
Treat stubborn vaginal yeast infections with an anti-fungal cream. Vaginal yeast infections can be treated with anti-fungal creams, ointments and vaginal suppositories. Examples of these treatments are miconazole (Monistat 3) and terconazole (Terazol 3). Your doctor can prescribe them or they are available (in weaker doses) over-the-counter at your pharmacy.
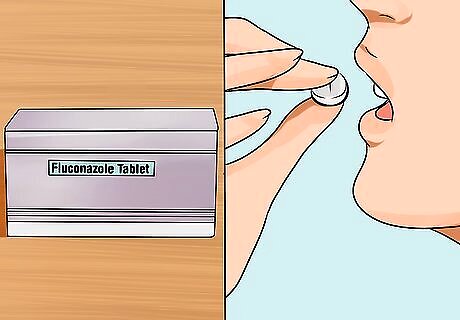
Treat a long-lasting yeast infection with fluconazole. Vaginal yeast infections can also be treated with a single oral dose of fluconazole (Diflucan). Recurrent or more complicated yeast infections may be treated with higher doses of the medications or you may be asked to take them for a longer period of time. Most often, your partner won’t need treatment. However, this may change if you experience recurrent infections.

Use caution if you are pregnant. Pregnant women can experience yeast infections, which should be cleared up before the baby is due. If you still have a yeast infection when the baby is born, it can pass to the baby, causing thrush. Check with your doctor about treating vaginal infections during this time.
Preventing Vaginal Infections
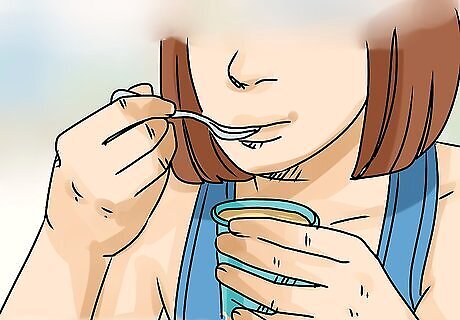
Take oral probiotics to prevent BV. You can take probiotics by mouth (either as capsules or in yogurt). These are mainly useful for prevention rather than treatment of BV. Yogurt can also be a good source of probiotics, as some types of yogurt have 90 to 500 billion Colony Forming Units (CFUs). Make sure to choose a yogurt that has this information on the label.

Wash your genital area gently. Use a very mild soap and warm water to wash your genital area. Dry yourself with a clean towel or allow yourself to air dry. You can also try drying it with a blow dryer set on cool. Avoid scratching or rubbing your genitals. Keep irritation at a minimum by leaving your genitals alone. Don’t scratch or rub the area.
Wear only 100% cotton underwear. Cotton allows your genital area to stay cool and dry. Avoid nylon, acetate, and any synthetic fibers. Avoid wearing thong underwear because these tend to be irritating.
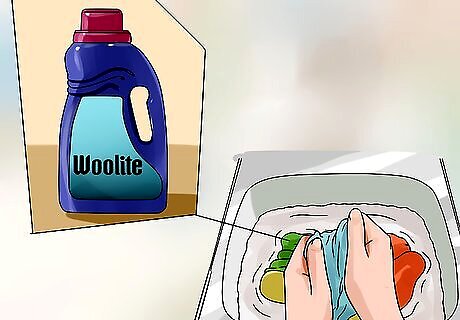
Use a mild detergent for your underwear. Use a mild and enzyme-free soap (such as fragrance-free Woolite) for washing your panties. Do not use fabric softeners or dryer sheets. These also contain chemicals that may irritate you. Double-rinse your underwear to ensure that all detergent is gone. Detergent residue can cause irritation.

Practice good habits with toileting. Use white, soft toilet tissue. Remember to always wipe from the front to the back to minimize the risk of infection from bowel bacteria.
Use unscented period products during the day. Instead of using scented napkins or napkins while you have your period, use unscented varieties. Replace tampons every few hours, depending on your flow. Do not leave tampons in overnight. Use sanitary pads instead.

Avoid wearing pantyhose. Tight clothing like pantyhose do not allow the genital area to “breathe.” They also trap heat and moisture, which creates the perfect setting for bacteria, yeast, and other organisms. Instead, wear nylons with a cotton panty insert.

Avoid irritating products. Avoid period products, which can irritate the vulva. These include deodorant sanitary pads, all vaginal sprays and deodorants, and any products with added perfumes. Avoid bubble baths, bath oils, talc, or powder, especially powder that contains cornstarch. Cornstarch provides food for microorganisms.
When Should You Try This?

Treat vaginal infections after getting diagnosed. While some vaginal infections can be cured without the use of medications, it’s important to consult your OB/GYN or primary physician before beginning any treatment. Since some symptoms are common among multiple types of vaginal infections, self-diagnosis is both difficult and risky. An official diagnosis from your doctor is the only safe way to identify the type and degree of vaginal infection you have. Tell your doctor if you have a strong preference for natural remedies. Some doctors are willing to work with you to accommodate this preference, and they should be able to guide you on which remedies would be best to try for your specific needs. Note that trichomoniasis is technically an STI. Natural remedies will not be sufficient to cure an infection caused by trichomoniasis; you will need medication to treat it.
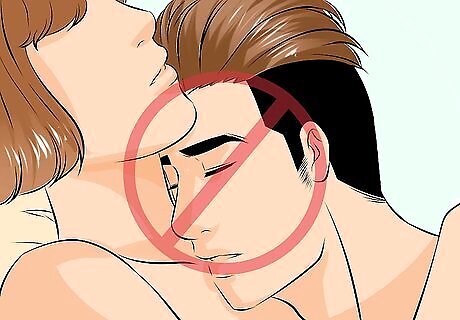
Try natural remedies if you can limit or abstain from sexual activity during treatment. Abstaining from sexual activity may not be necessary for all treatments, but you should check with your doctor or do some thorough research to determine if the remedy you’ve chosen is safe for you and your partner before engaging in sexual activity during treatment. In particular, exercise extreme caution when taking boric acid suppositories. Boric acid is toxic when ingested, making oral sex especially dangerous.
















Comments
0 comment