
views
X
Trustworthy Source
PubMed Central
Journal archive from the U.S. National Institutes of Health
Go to source
We’ll walk you through the entire process of receiving medical TCA treatments, then answer several common questions you probably have. Read on so you can feel confident about treating your warts with TCA.
- TCA destroys an HPV wart through a series of weekly applications. While the treatment is straightforward, it should only be done by your doctor.
- TCA usually causes some temporary pain when applied to a wart, but most patients tolerate it well. It has few if any other common side effects.
- Your doctor might recommend other topical medications, surgical removal, or a wait-and-see approach for your HPV warts.
- Vaccination, avoiding contact with warts, and practicing safe sex are the best ways to avoid developing HPV warts.
Getting Medical TCA Treatments
Discuss TCA with your doctor and get your questions answered. When administered by a medical professional, TCA is generally safe and effective in treating HPV warts. That said, the treatment itself can be somewhat painful, and it may take several weekly visits to achieve the desired result. So have an honest two-way conversation with your healthcare provider about the potential pros and cons of using TCA. In deciding whether or not TCA is an appropriate treatment in your case, your doctor may ask you questions like how long you’ve had the warts, if you’ve had HPV warts before, what treatments (if any) you’ve used before, whether the warts cause you physical pain or discomfort, and if the warts are causing emotional distress. In turn, you might ask questions like: How did I get these warts? What are my treatment options? How does TCA work? Is it painful? Is there any danger in leaving HPV warts untreated?
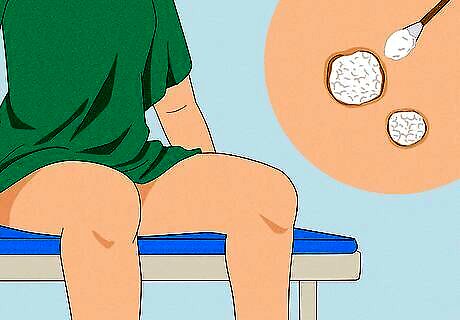
Undergo the treatment at your doctor’s office. TCA application is pretty straightforward: You’ll sit or lie down so that the treatment area is easily accessible to your doctor. They will lightly dab or brush a very small amount of the TCA (which has a thin, water-like consistency) onto the wart(s). You’ll then be asked to remain seated or lying down until the TCA dries and a white frost-like film appears on top of the wart(s). Do your best to remain completely still while your doctor applies the TCA. The treatment will go much more smoothly if none of the TCA ends up on your surrounding skin.

Alert your doctor to your pain level during the treatment. It is normal to feel pain, heat, and discomfort as the TCA does its job. Your doctor may cover the HPV wart in a light film of lubricating jelly to minimize the pain. The amount needed will vary with the size of the affected area. Your doctor may also neutralize the TCA if the pain is intense. TCA is a strong acid and can cause serious tissue damage if it is misused. If you feel intense pain when the TCA is applied, tell your doctor right away. They can neutralize the acid by covering the area with sodium bicarbonate (baking soda) or talcum powder. In most cases, the pain you feel during a treatment will only last for a few minutes, and rarely for as long as thirty minutes.
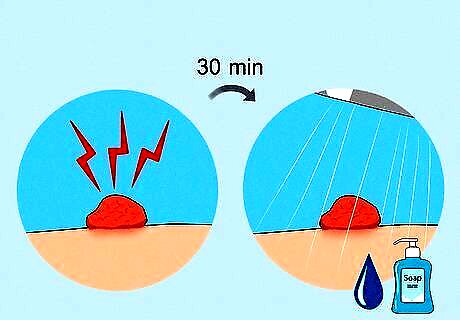
Manage post-treatment discomfort and watch for complications. If you continue to feel pain for more than thirty minutes after the TCA treatment, wash the area with soapy water and contact your physician. If the skin surrounding the wart becomes crusty or starts oozing, contact your physician immediately. Some patients experience a temporary change in the color of the skin on or around the area where TCA was applied—this is not a cause for concern.
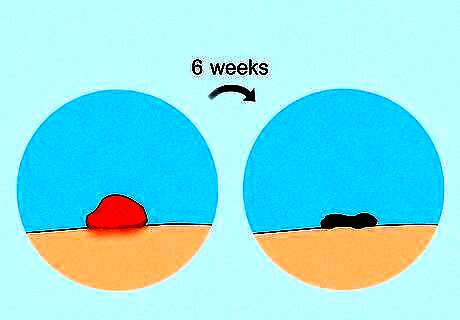
Monitor your wart's condition. Check the area every day or two and look for signs of improvement. The wart may start to shrivel and/or turn black within a few days, or it may look essentially the same as before. It’ll almost certainly require at least six weekly treatments to eliminate a wart with TCA, so don’t get discouraged if you don’t see quick results. Wash the area as normal between treatments. While checking on the status of your treated wart, keep an eye out for the appearance of new warts as well. TCA does not treat the underlying HPV that causes warts, just the warts themselves.
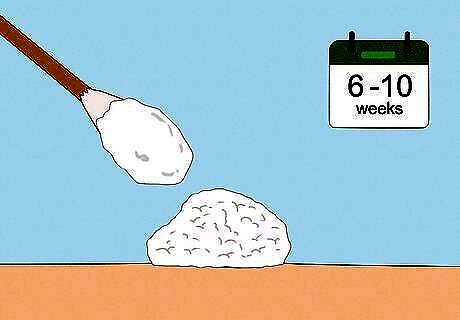
Return to your doctor's office for follow-up treatments. Each week, return to the doctor for an application of TCA. A treatment schedule usually lasts for six to ten weeks. If you don’t see significant progress after about six weeks, it may be time to consider other treatments. Talk to your physician if you’d like to switch to another option. With each treatment, the wart will continue to shrivel up until it eventually falls off, revealing a pale patch of skin underneath. The pale skin should return to normal over a period of a few weeks to a few months.
I found TCA for sale online—can I self-treat my wart?
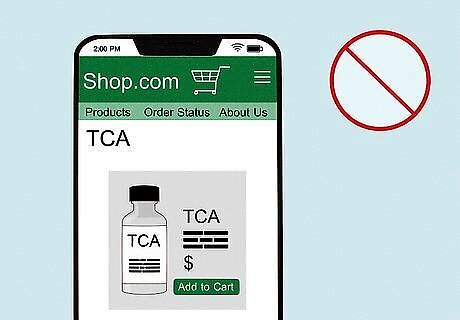
Please don’t—TCA can cause significant pain and skin damage. TCA is thin like water, so it’s very easy to get it on the skin surrounding your wart—if this happens, you’ll feel a strong burning pain and may end up with tissue damage that requires medical care. Avoid this risk by getting your TCA treatment by a trained professional in a medical setting. Here’s another reason not to use TCA you buy online: How can you be sure that it’s really TCA (at the listed strength) in the bottle? If you do self-apply TCA and you do (inevitably) get it on your surrounding skin, immediately apply baking soda to neutralize the acid.
What options other than TCA might my doctor recommend?

They may recommend topical meds, surgical removal, or no treatment. While TCA is a common option, there are a wide variety of treatments available for treating HPV warts. Your doctor will consider the size, shape, location, and quantity of warts, as well your discomfort level (both physical and emotional) and the cost of the various treatments. Common options other than TCA include: Self-administered medications. These topical treatments include options like podofilox, imiquimod, and sinecatechins. Follow your doctor’s application instructions carefully. Podophyllin resin. Your doctor will apply this as weekly as needed. Cryotherapy. This is the process of freezing off the warts using liquid nitrogen or a cryoprobe, possibly over several treatments. Laser removal. Warts are essentially burned away by your doctor using a high-powered laser. Surgical removal. This option is usually reserved for single larger warts or bigger clusters of warts. No treatment. HPV warts often disappear on their own, sometimes over a period of a few weeks to a few months.
How can I reduce my risk of getting HPV warts?
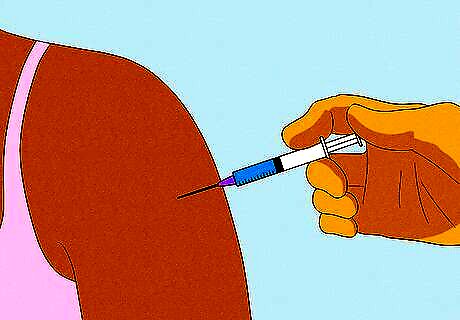
Get vaccinated against HPV. Gardasil 9, which is the only HPV vaccine currently in use in the United States, helps protect against the strains of HPV that cause genital warts as well as those that can cause cervical cancer. Vaccination is recommended for everyone ages 9-26, and on a case-by-case basis for those ages 27-45. Depending on your age and other factors, the vaccine will be given as a series of two or three shots. Vaccination does not treat HPV if you already have it, but it is very effective at preventing HPV infection.
Avoid contact with other people’s warts. This includes sexual contact, but also any other type of direct physical contact. In addition, you should not share towels or clothing with someone if those items may have come in contact with their HPV warts.
Use a condom during sex. While you should avoid sexual contact with someone who currently has HPV warts, using a condom can reduce (but not eliminate) the risk of getting HPV from someone who does not currently have warts. Using condoms also lowers your risk of spreading a range of other sexually-transmitted infections (STIs).
















Comments
0 comment