views
- Exercise at least 3 times a week for about 30 minutes to reduce inflammation.
- Eat berries, spinach, almonds, salmon, and other anti-inflammatory foods regularly. Use anti-inflammatory herbs like oregano and cayenne in your cooking.
- Support your diet and exercise by staying hydrated and taking any prescribed medications from your doctor.
- An elevated or high ESR can be a symptom of another condition. Along with your initial ESR test, work with your doctor to take other tests to get a diagnosis.
Home Treatments to Lower ESR

Exercise regularly and vigorously if you’re able. Vigorous exercise gives you a high-intensity workout that helps lower your ESR. Whichever activity you choose, make sure it makes you sweat, elevates your heart rate, and leaves you thinking, “Wow, this is tough!” Aim to work out for a minimum of 30 minutes at least 3 times per week. Studies show that vigorous exercise significantly reduces inflammation. Some vigorous exercises include running, going for a fast bike ride, swimming laps, doing aerobic dancing, or hiking uphill.
Do light to moderate exercise as an alternative. If you’ve never really exercised before or have a condition that keeps you from doing vigorous activity, go for a lighter workout. Choose an activity that lasts at least 30 minutes. Just moving a little bit each day helps bring down your inflammation. Push yourself until you feel like you’ve reached the point of, “Ok, this is hard, but I’m not struggling yet.” For example, go for a walk around the block at a brisk pace or sign up for a water aerobics class.

Do 30 minutes of yoga nidra each day. Yoga nidra is a type of yoga practice that involves suspending yourself between wakefulness and sleep. It helps to relax you both mentally and physically. In at least 1 study, researchers found that this type of yoga significantly reduced elevated ESR. To do yoga nidra: Lie flat on your back on a mat or other comfortable surface. Listen to the voice of your yoga instructor. If you don’t have a yoga studio that offers nidra, download a yoga app or find an audio recording or video online. Allow your breath to flow naturally in and out of your body. Do not move your body during the practice. Allow your mind to float from point to point, staying aware without concentrating. Achieve “sleep with a trace of awareness.”

Avoid processed, sugary foods. These foods contain a harmful type of cholesterol, called low-density lipoprotein or LDL, that can cause inflammation in the body. This inflammation may also raise your ESR. In particular, avoid french fries and other fried food, white bread, pastries, soda, red and processed meat, and margarine or lard.
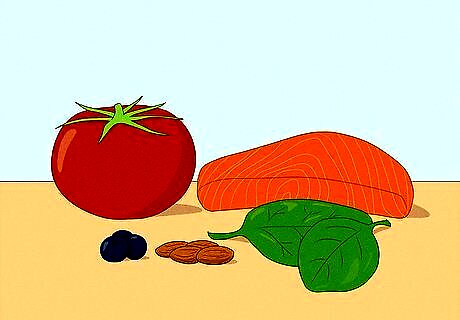
Eat lots of fruits, veggies, nuts, and healthy oils. These options help you eat healthy, along with lean meats like chicken and fish. While eating more fruits, veggies, and healthy oils improves your health, specific types also reduce inflammation. Incorporate these foods into your meals several times a week: Tomatoes. Strawberries, blueberries, cherries, and oranges. Green leafy vegetables like spinach, kale, and collards. Almonds and walnuts. Fatty fish with a high oil content like salmon, mackerel, tuna, and sardines. Olive oil.
Add herbs like oregano, cayenne, and basil to your cooking. These ingredients naturally fight inflammation in the body, so incorporate them into your meals whenever you can. Luckily, using herbs is a great way to spice up your meal plans (pun intended)! Ginger, turmeric, and white willow bark are some more tasty species that help reduce inflammation and your ESR. Look up recipes online that use these herbs. For ginger and willow bark, use a tea infuser to make herbal tea. Do not take willow bark if you’re pregnant or breastfeeding.

Drink plenty of fluids each day. While being dehydrated may not worsen your inflammation, hydration is crucial to avoid muscle and bone damage. Given that you’re ramping up your activity level to bring down inflammation, it’s important to drink water to prevent injury. Shoot for at least 1 to 2 litres (0.26 to 0.53 US gal) of water each day. If you’re experiencing any of the following symptoms, drink some water right away: Extreme thirst Fatigue, dizziness, or confusion Less frequent urination Dark-colored urine
Understanding Your Test Results
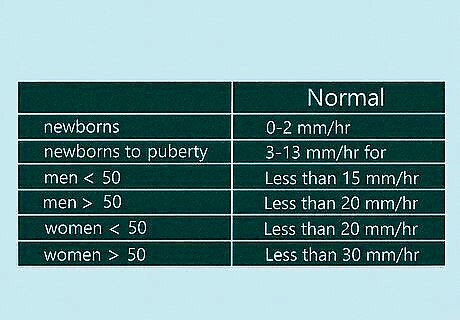
Talk to your doctor to understand your test results. Just like most laboratory tests, the normal ESR ranges can depend on which lab your doctor uses. Sit down with your doctor when you get your results to talk through them together. In general, normal ranges are: Less than 15 mm/hr (millimeters per hour) for men under 50. Less than 20 mm/hr for men over 50. Less than 20 mm/hr for women under 50. Less than 30 mm/hr for women over 50. 0-2 mm/hr for newborns. 3-13 mm/hr for newborns to puberty.
Ask your doctor if your ESR is elevated or very high. There are several conditions that can elevate your ESR, including pregnancy, anemia, thyroid or kidney disease, or cancers such as lymphoma or multiple myeloma. A very high ESR is sometimes associated with lupus, rheumatoid arthritis, or a severe infection in your body. A very high ESR might also be a symptom of rare autoimmune disorders like allergic vasculitis, giant cell arteritis, hyperfibrinogenemia, macroglobulinemia, necrotizing vasculitis, or polymyalgia rheumatica. Infections associated with a very high ESR are often in your bones, heart, on your skin, or throughout your body. It can also be a sign of tuberculosis or rheumatic fever.
Take other tests to get a diagnosis. An elevated or high ESR can be a symptom of several different diseases, so it’s important to remember that your ESR itself isn’t a diagnosis. Your doctor will perform other tests to understand what’s going on in your body. While you wait for your doctor to determine which tests you need, take a deep breath. Surround yourself with a support system and discuss your fears with your doctor, family, and friends. An ESR test doesn’t provide a diagnosis on its own.
Get your ESR tested regularly to monitor your levels. Because an elevated ESR is often associated with chronic pain or inflammation, your doctor will likely ask you to come in for regular check-ups. Monitoring your ESR during these routine visits allows them to keep an eye on your pain and the inflammation in your body. Hopefully, with the right treatment plan, you’ll see your levels going down!
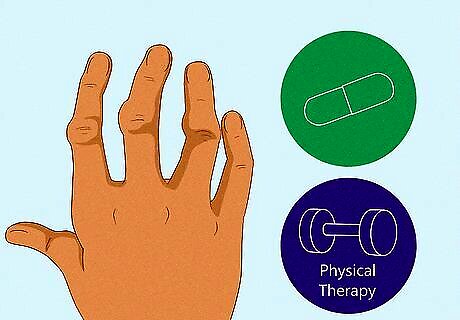
Manage rheumatoid arthritis symptoms with meds and physical therapy. Unfortunately, rheumatoid arthritis can’t be completely cured. However, it is possible to manage the symptoms and go into remission. Your doctor might prescribe a combination of disease-modifying antirheumatic drugs (DMARDs), nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, and steroids to do so. Physical or occupational therapy teaches you exercises to keep your joints moving and flexible. They also teach you alternative methods for doing daily tasks, like pouring yourself a glass of water, in cases of extreme pain.
Help control lupus flare-ups with NSAIDs and other meds. Every case of lupus is different, so work with your doctor to find a course of action that is best for you. NSAIDs can help manage pain and fever while corticosteroids can control inflammation. Your doctor may also recommend antimalarials and immunosuppressants, depending on your symptoms.
Address bone and joint infections with antibiotics and/or surgery. Elevated ESR can be associated with several infections, but they most commonly point to infections in the bones or joints. These infections are particularly difficult to treat, so your doctor will likely ask you to do other tests to determine the type and source of the problem. In serious cases, they may need to do surgery to remove the infected tissue.
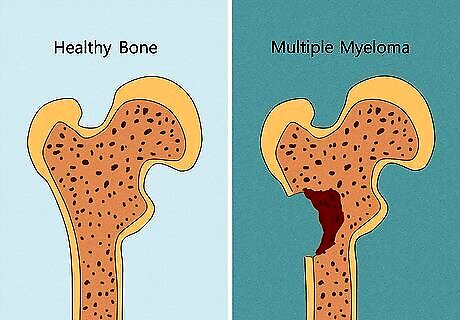
Get a referral to an oncologist if you’re diagnosed with cancer. A very high ESR above 100 mm/hr can sometimes indicate malignancy. This is the presence of cells that invade nearby tissues and spread cancer. In particular, high ESR may point to multiple myeloma, or cancer in the bone marrow. If you are diagnosed with this condition using other blood tests, as well as scans and a urine test, work with an oncologist to develop a specialized treatment plan.
Getting an ESR Test
Visit your doctor if you think you need an ESR test. An ESR test determines if there’s inflammation in your body that’s causing you pain. If you have unexplained fevers, arthritis, muscle pain, or visible inflammation, an ESR test can help your doctor better understand the source and severity of these issues. An ESR test is often useful in diagnosing unexplained symptoms like a poor appetite, unexplained weight loss, headaches, or shoulder and neck pain. An ESR test is rarely done on its own. Doctors typically ask you to take a C-reactive protein (CRP) test too. This test is also checks for inflammation in the body.
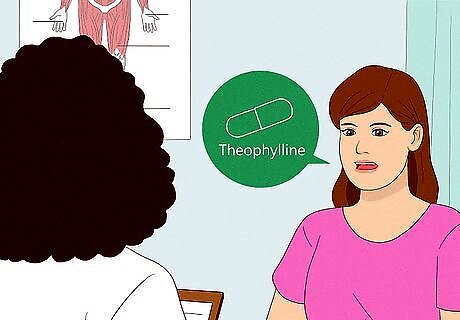
Discuss any medications you’re on with your doctor. Some over-the-counter and prescription drugs can elevate or lower your natural ESR. If you’re on any of these meds, your doctor may ask you to stop taking them up to 1 week before you take the test. Do not change your medications without consulting your doctor. Dextran, methyldopa, oral contraceptives, penicillamine procainamide, theophylline, and vitamin A can increase ESR. Aspirin, cortisone, and quinine sometimes lower your ESR.
Tell the health professional which arm you want blood drawn from. Healthcare professionals typically draw blood from the crook of your elbow. Prepare for your blood test by thinking about the best arm to use. While there’s usually not much pain or swelling after the test, ask the health care profession to use your non-dominant arm. Your healthcare professional will try to honor your preference, but they’ll also look for the best veins to use on either arm. Choosing a good vein helps the test to go a bit faster. If your health professional can’t find a good vein in either arm, they may look for another spot to draw from. Tell your healthcare professional about your past blood draw experiences. If you experience faintness or lightheadedness during blood draws, they may ask you to lay down to make you comfortable and keep you from getting hurt. If you don’t do well with blood tests, ask a friend or family member to take you to and from the test.
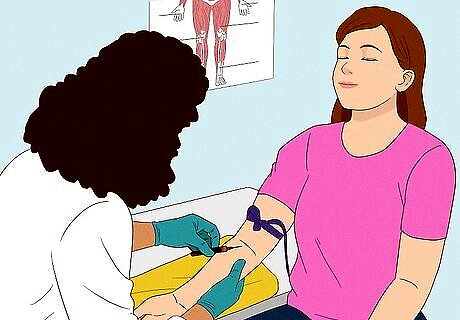
Remain relaxed while your blood is drawn. Knowing what happens during a blood draw can help you feel less nervous about needles. Before the test, the healthcare professional usually ties an elastic band around your upper arm and swabs the draw site with alcohol. Then, they insert a needle into your vein and draw your blood into a tube. When they’re done, they remove the needle and release the elastic. Finally, the nurse or doctor typically gives you a small gauze pad to put pressure on the spot. If you’re nervous, don’t look at your arm while your blood is being drawn. Depending on your test, your healthcare profession may fill more than one tube. Ask your blood drawer before hand to know how much blood they’ll take. Some offices give you a compression bandage to apply pressure to the spot and stop the bleeding. You usually remove this bandage at home a few hours after your appointment.
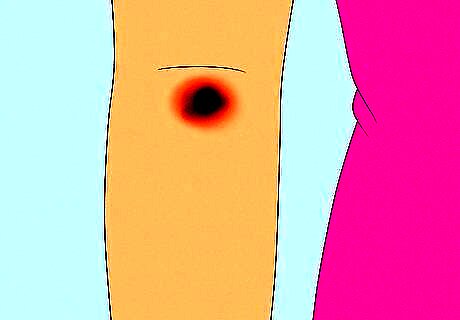
Expect some bruising or redness around the area of the blood draw. In most cases, the blood draw site heals in 1 to 2 days, but it may appear a bit red or even bruised as it’s healing. This is normal. In rare cases, the vein used for the test may become swollen. This isn’t serious, but it might be painful. If you feel pain, ice the area on the first day, then move on to a warm compress. Make a warm compress by heating a damp washcloth in the microwave for 30-60 seconds. Apply it to the site in 20-minute sessions a few times per day. Test the washcloth’s temperature by hovering your hand over it. If the steam coming off the cloth is too hot for you to hold your hand above it, wait 10-15 seconds before testing the temperature again.

Contact your doctor if you develop a fever. If the pain and swelling at the blood draw site gets worse, an infection might be the cause. This is a very rare reaction. Take your temperature to determine if you have a fever. If you do, contact your doctor right away. If you have a fever of 103℉ (39℃) or higher, your doctor may tell you to go to the emergency room.
















Comments
0 comment