views
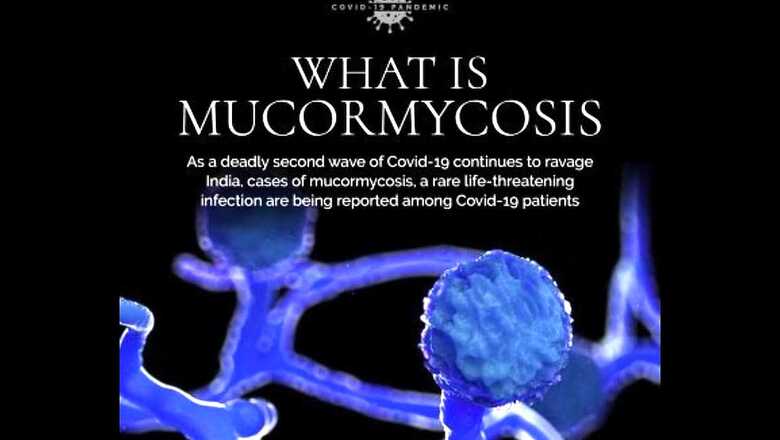
If black fungus had emotions, it would have been pained and hurt. For much of May, black fungus was blamed for a disease condition which it never caused. As if the devastating second wave of COVID-19 was not enough, starting early May, reports of a new health condition with symptoms of fever—headache, cough, pain and redness around eye and nose—shortness of breath, black discolouration over nose, alternation in mental status such as confusion or forgetting things and even bloody vomit started doing the rounds. A number of patients with COVID-19 were suffering from this condition.
It is difficult to ascertain whether it was the black discolouration over nose or the appearance of black dots over the culture media between the colonies of fungal growth that the disease and the causative agent started being termed as black fungus.
The fact remains that although it is a fungal disease, it is not caused by black fungus. The fungal disease reported during the second wave of COVID-19 in India is mucormycosis (also called zycomycosis), caused by a group of fungi named mucormycetes.
What are fungi?
Fungi are organisms that include a wide range of subgroups including yeasts, molds and even mushrooms. In biological classification, they are grouped differently from plants, animals and protozoa etc. Fungi are nearly ubiquitous and most of them are harmless, and they are all around us—some reside in the damp walls of our houses, some in plants, soil, fallen leaves as well at construction sites. However, we don’t have to worry. In a healthy person, the immune system is well designed to fight these fungi and guard against any illness.
What is the difference between black fungus and mucormycetes?
The black fungus is also known as black yeast and is a slow-growing, pigment-producing fungi. Very rarely do they cause illness after skin trauma or through inhalation, especially in those who already have medical conditions such as cystic fibrosis. Mucormycetes, the causative fungi for the infection in second wave of COVID-19 pandemic, are different and have the ability to infect the sinuses (especially those in nose and face) and also gastrointestinal tract and even brain.
How big is the mucormycosis problem?
Even before COVID-19 pandemic, cases of mucormycosis were reported at an estimated rate of 14 per 100,000 every year. A few studies have reported that between July and December 2020, there was a slight increase in mucormycosis cases in India; however, during the second wave, there was a rapid increase and India reported a total of around 11,000 such cases. Mucormycosis was declared an epidemic.
Is every COVID-19 patient at risk of mucormycosis?
Let’s put this in perspective. Between April 1 and May 31, India reported 1.6 crore COVID-19 cases. The number of mucormycosis cases reported during this period was around 11,000. Clearly, the cases of mucormycosis are just a fraction of the total COVID-19 cases; however, the disease is more severe when reported in a COVID-19 patient, with up to 50 per cent mortality rate. That is one of the reasons it was declared an epidemic, to mount an urgent response.
Mucormycosis, wrongly reported as black fungus, has created some level of panic and fear among people. However, we need to remember that every person who tests positive for COVID-19 is not at risk of developing this rare infection.
So, who is at risk of developing mucormycosis?
A select sub-group of people are at a higher risk of mucormycosis. These include people with uncontrolled diabetes mellitus; those with immunosuppressed status, like those with HIV or on cancer therapy or steroid therapy; with sustained and prolong ICU stay; with co-morbidities and post-transplant/malignancy etc.; and with primary immunodeficiency (in other words, those with known medical condition which results in weaker immunity).
It also needs to be remembered that steroids are an integral part of COVID-19 management, especially for moderate and severe illnesses. However, its excessive or long-term use can increase the risk of an individual becoming prone to fungal and other infections. Steroids are also known to result in reduced blood sugar control, which makes people susceptible to secondary infection.
When to suspect mucormycosis?
This condition is more commonly reported in those with moderate to severe COVID-19 illness. There is no need to panic and the risk of a healthy person or even someone with mild COVID-19 infection getting mucormycosis is rare. However, to ensure that we are prepared, anyone who has reported the above-listed risk factors should be alert. A few warning signals should not be missed:
* Pain and redness around eyes and/or nose, fever
* Nasal blockage or congestion, nasal discharge (blackish/bloody), local pain on the cheek bone
* One-sided facial pain, numbness or swelling
* Blackish discolouration over bridge of nose and/or palate
* Toothache, loosening of teeth, jaw involvement
* Blurred or double vision with pain; fever, skin lesion; thrombosis and necrosis
* Chest pain, breathlessness, bloody vomiting; worsening of respiratory symptoms
* Altered mental status, such as confusion or forgetting things
If you show any of these symptoms, consult your doctor and healthcare provider immediately.
How can mucormycosis be treated?
There are medicines, particularly the antifungal Amphotericin B, that are being used to treat mucormycosis. In severe cases, surgery of the affected part may be needed. However, as part of clinical case management, strict control of blood sugar levels and reducing the use of steroid or other immunosuppressant drugs (which the patient might have been using for other health conditions) are needed. The antifungal therapy is needed for at least 4-6 weeks and the patient would require hospitalization and management by a multi-disciplinary team of doctors. No attempt should be made to manage the patient at home.
Prevention is always better than cure
Since we have learnt about mucormycosis in last few weeks, we should make every possible effort to prevent the infection. Masks are must when stepping out, especially if you are visiting places that are dusty. This becomes excessively important for those who have recovered from COVID-19— moderate to severe illness— as well as anyone with above-listed risk factors. Wear shoes, long/full trousers, long-sleeve shirts and gloves while handling soil (gardening) or manure or plant leaves etc. It is important to keep blood sugar in check—monitor the levels regularly. Those using humidifiers during oxygen therapy should use clean, sterile water. It needs to be understood that there is no benefit in taking antifungal medicines before a person develops the condition (often termed prophylaxis).
It is equally important to remember that those at high risk should pay attention to any warning sign and symptom; should not delay and seek immediate consultation, if required.
White, orange and yellow fungi: Ignore the colour
There are fungi in as many colours we can imagine. The colour of the fungus is immaterial and not linked to the severity of the disease. Therefore, when fungal illnesses were being reported by colours, it was irrelevant.
What next?
We need to examine the rapid increase in cases of mucormycosis in May 2021 from a public health perspective. Scientific and epidemiological research is needed to find the reason for the sharp rise in cases. Now, with the COVID-19 second wave on decline, it is likely that cases of mucormycosis will also come down. However, to be prepared, we need to empower ourselves with the right information. Remember, the risk of mucormycosis in a healthy person is very low, far lower than many other diseases. Do not panic; if identified early, it can be treated.
Read all the Latest News, Breaking News and Coronavirus News here.



















Comments
0 comment