
views
Determining the Degree of Your Burn
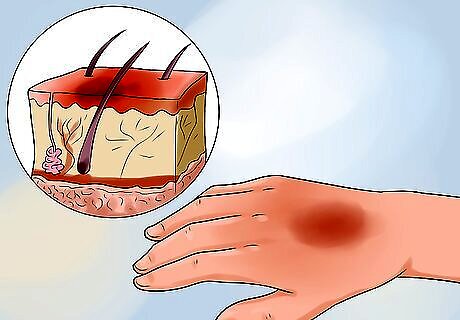
Figure out if you have a first degree burn. First degree burns are the most common, and happen as a result of light scalding, brief contact with hot items, and the sun. The damage is only on the most superficial or outer layer of the skin.They will likely appear red, slightly swollen, and may or may not be slightly painful. Treat your first degree burn at home, since there is usually no need for expert medical attention. The outermost layer of skin has the ability to heal itself with care and time. First degree burns are classified as ‘minor burns’ and should be treated as such. Sometimes you may get an extensive first degree burn, such as a full body sunburn, but this does not need medical attention.
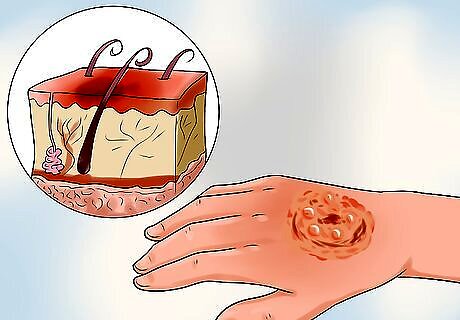
Know if you have a second degree burn. Your skin might also appear blotchy, blisters will form, and the pain will be much more intense. Second degree burns come from brief contact with incredibly hot things (boiling water, for example), extended contact with hot items, and prolonged exposure time in the sun. Unless your second degree burn is on your hands, feet, groin, or face, treat it like a minor burn. If you have blisters, don't drain them. If the blister is drained, keep it clean by rinsing with water and swabbing with antibacterial ointment. You can also cover the ointment on the skin with a bandaid or another dressing. This dressing needs to be changed daily. A second degree burn burns through two layers of your skin. If your second degree burn is wider than three inches, covers your hands, feet, joints, or genitals, or doesn't heal over several weeks, then you should call your doctor for medical help.
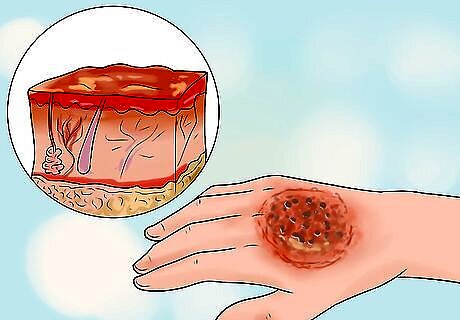
See if you have a third degree burn. Third degree burns are the most serious and need immediate medical attention. These happen when extended exposure to a hot object burns through all three layers of your skin, sometimes causing muscle, fat, and bone damage. The burns will look leathery and have a white or black appearance. The pain can vary depending on the level of damage to the nerves in the skin layer (pain receptors). These burns can look “wet” because of the rupture of the cells and protein leakage. Third degree burns are always classified as a major burn and need treatment from a doctor as soon as possible.
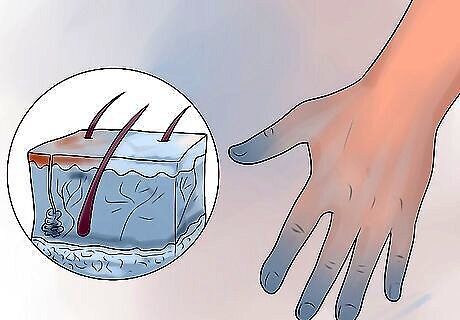
Check low-temperature burns. These are ‘burns’ that occur when your skin is exposed to low temperatures, like snow or ice, for an extended period of time. The area will look bright red, white, or black and will have a strong burning sensation as the skin is rewarmed. A low temperature “burn” is still considered a burn because it damages the skin's tissue layers. Treat low-temperature burns as major burns in most cases, and get medical help for treatment. Rewarm the skin in 37°C/98.6°F to 39°C/102.2°F water immediately after exposure.
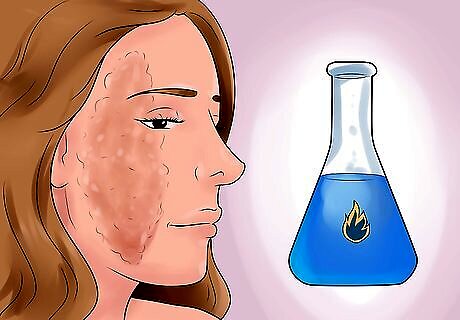
Determine if you have a chemical burn. Chemical burns are another type of burn caused by skin contact with harmful chemicals that damage the skin layers. These types of burns will probably appear in the form of red patches, a rash, blisters, and open sores on your skin. Your first step is always to determine what caused the burn and to call poison control immediately. Contact a poison control center immediately if you believe you've suffered a chemical burn. Care must be taken to neutralize and isolate the spread of the chemical. Irrigate chemical burns with lots of water, however, avoid water if exposed to dry lime or elemental metals (such as sodium, magnesium, phosphorus, lithium etc.) as these can react with water and cause more injury.
Treating Minor Burns

Run cool water over the burn. As soon as you can, run cool water over the burn. This will prevent further damage to your skin. Stick the burned area under cool running water for 10-15 minutes or until the pain subsides. Avoid using cold water, since this can damage the skin around the burn. The sudden shock of extreme heat to extreme cold will only slow the healing process.

Remove tight clothing or jewelry quickly. As soon as you can, or while rinsing the burn, remove anything that might constrict your skin as the wound swells. When in doubt, take it off. This lets blood to flow to the wound and starts healing it. Removing tight clothing or jewelry can also prevent further damage.

Apply a cold compress. If cold water isn’t an option, use a cold compress or ice pack wrapped in a towel. Place it over your burn. Apply the compress for 10-15 minutes, wait for 30 minutes, and then reapply for 10-15 minutes. Never apply ice or your compress directly to the burn, since this will damage the skin. Keep the towel between you and the ice instead.

Take an over the counter pain reliever. An over-the-counter pain reliever such as ibuprofen, acetaminophen, aspirin, or naproxen can be helpful if the symptoms are bothering you. If the pain does not lessen after several hours, take another dose of the medication. Avoid giving aspirin to young children or if you are recently recovering from the flu or chickenpox. Follow the specific package instructions. They'll be different depending on what medication you choose.

Clean the burn. After washing your hands, use soap and water to clean the burn and prevent infection. Apply an antibiotic like Neosporin when you are done to keep the burn clean. Aloe vera can also soothe your skin. Look for aloe vera with few additives. Antibiotics or aloe vera can also keep the bandages from sticking. Do not pop blisters while you clean since they actually protect your skin from infection. Take care not to pop the blister or drain the contents, since the body is able to take care of minor blisters on its own. Antibiotic ointment isn't needed if your blisters haven't popped. But, if they have or if your wound is exposed, use an antibiotic to prevent infection.

Lightly cover the burn with ointment and then gauze. You may not need to apply a bandage to first degree burns, blisters that haven't popped, or skin that isn't exposed. But small second degree burns will need a wrap to keep out infection. Cover the burn lightly with gauze and secure it softly with medical tape. Change the gauze daily. Do not apply gauze directly to any wound. A wound must always be covered with a cream or ointment before applying gauze. Otherwise, when the gauze is removed, all the newly formed skin will be torn off with it. Remove gauze in the direction of surrounding hair growth. If the gauze is sticking to the wound, use lukewarm water or a saline solution applied to the stuck gauze for easier removal. Make a saline solution by adding 1 teaspoon of salt to a gallon of water.

Avoid using home remedies like egg whites, butter, and tea. The internet is awash with "miracle" solutions for burns, but few scientific studies have actually proven them to work. Many reputable sources, such as the Red Cross, found them to be worse for burns because they contain bacteria that can lead to infection. Natural moisturizers such as aloe vera or soy may be helpful in cases of sunburn and tanning bed burns.

Watch the burn for infection. Keep an eye on the wound for changes in color to red, brown, or black. Also, watch for any green discoloration of fat layers under and around the wound. Seek medical attention if a burn does not heal over several weeks. A burn that refuses to heal can be a sign of complications, infection, or a more serious burn. Let your doctor know if you experience any of the following signs: Signs of an infection include: warmth, tenderness, hardening of the wound area and fever greater than 39°C/102.2 F or less than 36.5°C/97.7 F. Seek immediate medical attention if your temperature falls within these ranges.

Alleviate itching with topicals. Itching is a common complaint among patients during the initial healing period after minor burns. Topicals such as aloe vera or petroleum based jelly can soothe the discomfort caused by itching. Oral antihistamines can also be taken to help with the itchiness.
Treating Major Burns

Call emergency services immediately. Don't try to treat major burns at home. They need immediate treatment by a professional. Immediately call for an ambulance or visit your doctor or an emergency room immediately. Never try to treat a serious burn yourself. The following measures are simply proactive steps to take until medical help arrives.

Safely remove the victim from the heat source. If possible, do whatever you can to prevent further burns or injury. Stop the heat source or move the suffering person. Never pull on or move someone using the burned area for leverage. If you do, you could further damage the skin and possibly open up a wound even more. This can cause great pain to a suffering victim and lead to shock.

Cover the burn. Apply a cool, moist towel over the burned area to protect it until help arrives. Do not use ice or immerse the affected area in cold water. This can cause hypothermia or further damage to the sensitive area.

Remove any chemical irritants. If your burn was caused by chemicals, clean the area of any remaining chemicals. Run the area under cool water or add a cool compress as you wait for emergency help. Do not attempt any home remedies on a chemical burn.
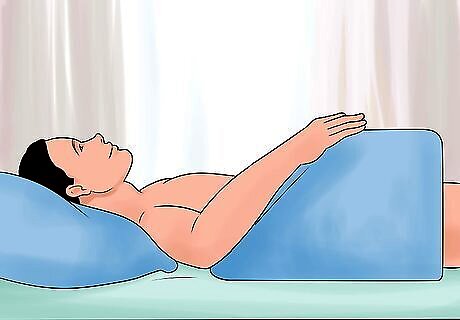
Elevate the burn above the victim's heart. Only do this if you can elevate the wound without causing further damage.

Seek immediate help for shock. Look for shock symptoms: weak or rapid pulse, low blood pressure, clammy skin, disorientation or unconsciousness, nausea, or combativeness. If you notice symptoms of shock from third degree burns, get medical attention immediately. Call an ambulance to get the victim to the hospital quickly. This is a life threatening situation on top of an already dangerous situation. Severe third degree burns can cause shock because the body loses a significant amount of fluids when a large surface area is burned. The body cannot function normally with such low levels of fluid and blood.
Treating Major Burns in Hospital Patients (for Health Professionals)

Remove clothing and jewelry. The victim may immediately be transferred from the hospital to a burn center for treatment. Then, remove any clothes or jewelry that are still on the victim if they might constrict the body, which might swell. The burn may cause so much swelling that certain parts of the body become dangerously compressed (compartment syndrome). If this happens, surgery might be needed to relieve the pressure. This would also help blood flow and nerve function.
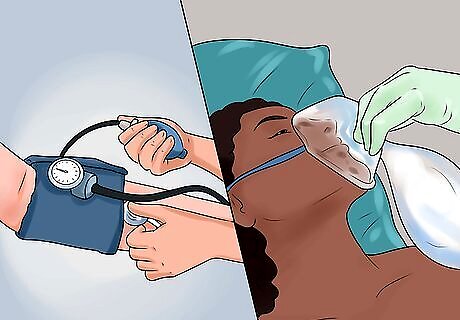
Take vital signs and give oxygen. For all major burns, the doctors may give 100% oxygen by intubation, a tube inserted in the windpipe. Vital signs are also immediately monitored. This way, the current state of the patient is assessed and a specific plan for care is made.
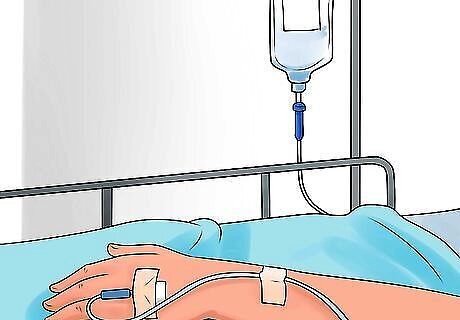
Re-hydrate the victim. Stop the loss of fluids and replenish the body of lost fluids with an I.V. solution. Determine the type and amount of fluid based on the individual's burn.

Give antibiotics and pain medications. Give pain and analgesic medication so the victim can better cope with the pain. Antibiotics are also crucial. Antibiotics are needed because the body's main line of defense against infection (the skin) has been compromised. Medication is needed to keep bacteria from entering and infecting the wound.
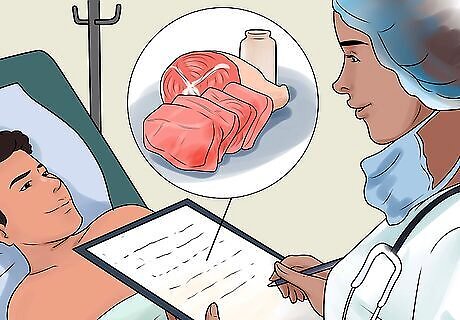
Adjust the patient's diet. Recommend a calorie-rich, high-protein diet. This helps to replenish the body with vital energy and protein needed to repair all the damaged cells from the burn. Foods that are rich in protein include: eggs, Greek yogurt, tuna, halibut, salmon, tilapia, steak (leaner cuts), boneless & skinless chicken breast, turkey breast, dried lentils, peanut butter, mixed nuts, tofu, wheat germ, and quinoa. High-calorie foods include: avocados, bananas, mangoes, whole wheat granola, whole grain bread, moderate amounts of corn

















Comments
0 comment